Eliminating Stethoscope Pathogen Transmission And Associated Costs

SAN DIEGO, Jan. 12, 2024 – Hand hygiene is practiced vigilantly across all national healthcare facilities, yet a lack of stethoscope hygiene may be undermining these diligent infection control efforts. A new clinical publication titled "The Hidden Expense of Stethoscope Hygiene vs the Real Costs of Failure," sheds light on the profound cost impact that suboptimal hygiene practices such as wiping with alcohol, substitution with disposable stethoscopes, and low hygiene compliance, can have.
The stethoscope, an integral tool in the healthcare setting, comes into direct contact with patients nearly as often as a clinician’s own two hands, and harbors a comparable diversity and volume of pathogens. It is now understood to be a potent and prominent vector of infection.
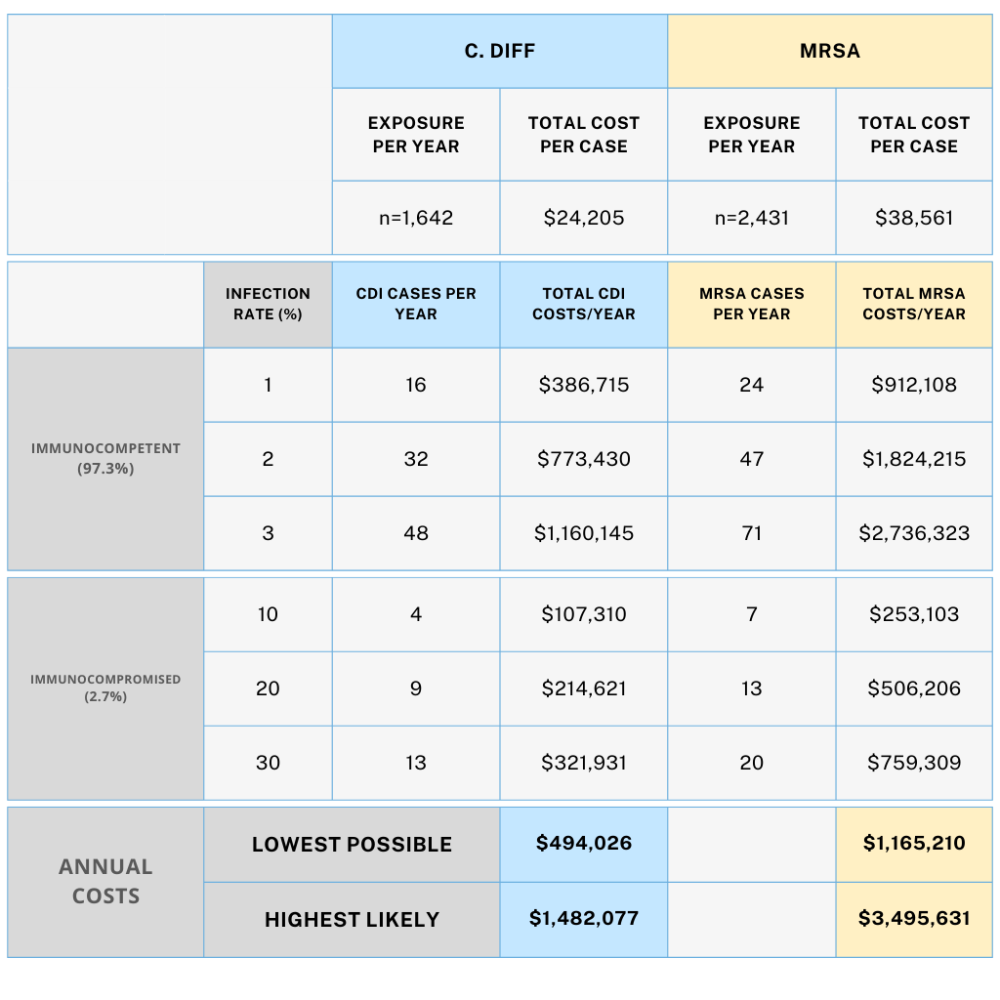
According to the study, a novel stethoscope hygiene product called The DiskCover System may enable clinicians to auscultate their patients without ever having to directly touch them with their stethoscopes again. Using an economic cost-savings sensitivity analysis model, the publication finds the adoption of touch-free, aseptic disk covers for stethoscopes can eliminate several healthcare facility costs. By reducing the costs associated with clinician time spent on stethoscope cleaning, potential healthcare-associated infections (HAIs), and purchase of ineffective equipment in disposable stethoscopes, hospitals can potentially save up to $5M annually.
Common stethoscope hygiene practices such as alcohol disinfection of the diaphragm, and use of disposable stethoscopes, have been demonstrated in a multitude of studies to be ineffective.
Alcohol cleaning is time-consuming, requiring up to 60 seconds of disinfection for maximum efficacy, which is a large restraint to high compliance. Even when done correctly, alcohol is incapable of killing all pathogens that can be found on the diaphragm, particularly alcohol-resistant organisms such as Clostridioides difficile. Meanwhile, clinicians widely agree that disposable stethoscopes do not work, with a study revealing a 10.9% misdiagnosis rate directly attributed to their use.
In response to these findings, the publication’s author, Dr. W. Frank Peacock, MD, FACEP, FACC, FESC, Professor and Vice Chair for Research in Emergency Medicine at the Baylor College of Medicine, advocates for a renewed focus on stethoscope hygiene protocols at both a national and regulatory level.
“Most recently, dispensers of touch free stethoscope barriers have been promoted as elevating stethoscope hygiene to that similar of the gloved hand and providing 100% aseptic patient contact,” said Dr. Peacock, “Ultimately, touch-free disk cover barriers may solve the failures of the unwashed personal stethoscope or the shared disposable stethoscope, and make it so the stethoscope never needs to directly touch a patient again – preventing any possible contact between the pathogens it harbors and the patient,” Dr. Peacock concluded.

The DiskCover System (www.diskcover.com) from AseptiScope Inc. ensures a touch-free patient auscultation via stethoscope every time and is proven to offer effective aseptic barrier protection, acoustic performance, time-savings, and workflow compatibility, all in a cost-effective, on-demand delivery system. The compact DiskCover System, designed to be mounted in or near hand hygiene stations in the clinical setting, applies individual disk cover barriers instantly, minimizing workflow disruption and encouraging clinician compliance.
