- The stethoscope has come under scrutiny as a vector for infection, particularly with the emergence of COVID-19
- A novel, aseptic barrier system from AseptiScope™ prevents pathogen transmission
June 29, 2020 San Diego, California – An article in the new issue of The American Journal of Medicine highlights the practical and symbolic importance of the stethoscope and its key role in assessment of COVID-19 patients. Despite continuous advances in the diagnosis of disease, the stethoscope remains a mainstay in patient evaluation in the 200 years since its invention. Today, given the respiratory dysfunction and cardiovascular co-morbid manifestations characteristic of COVID-19, the thorough assessment of patients with a stethoscope is critical, as is the need to maintain a pathogen-free stethoscope diaphragm surface. An automated, clinically validated and aseptic single-use barrier system from AseptiScope™ holds promise to fill a significant gap in stethoscope hygiene practices.
“The stethoscope is the most prominent and enduring symbol of the interaction and bond between the physician and the patient. This is even more important in the COVID-19 era,” said Alan Maisel, MD, Professor Emeritus at the University of California San Diego, co-author, and co-founder of AseptiScope, Inc. “The stethoscope is truly the clinician’s third hand and is at the heart of all physical examinations. Its ability to provide rapid diagnostic and prognostic information is unsurpassed.”
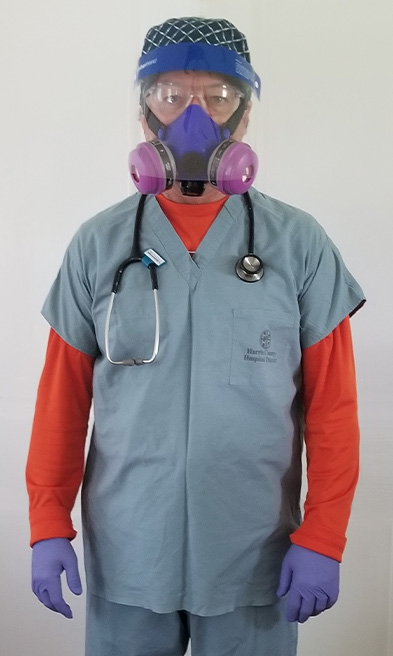
The authors point out that common pathogens found on clinicians’ hands are also likely present on their “third hand,” the stethoscope, and often at a significantly greater magnitude. In the light of the COVID-19 pandemic, current guidelines and practices related to stethoscope hygiene have understandably come into the spotlight. Current CDC guidelines call for stethoscope cleaning but fail to recommend a standard cleaning frequency, ranging from between-patients to once weekly. Given the reported ability of pathogens like COVID-19 to linger on surfaces, this lack of specificity for hygiene frequency may no longer be adequate. Moreover, despite CDC guidelines, the authors cite observational studies of clinicians in everyday practice that show a very low frequency of stethoscope cleaning, ranging from 13% to 24%.
“With the emergence of COVID-19, and in its wake, the difficulties in stethoscope hygiene have become disturbingly clear,” said Robert Gaynes, MD of the Division of Infectious Diseases at Emory University and co-author. “Just as clear is the persistent importance of the stethoscope and, so, the need to establish new approaches for its safe use.”
The authors emphasize that common stethoscope cleaning practices, such as alcohol wipes, bleach, and hydrogen peroxide, even when used effectively, produce mixed results in reducing pathogen transmission risk. Additionally, the authors cite studies finding that single-patient disposable stethoscopes offer compromised auscultation quality and present a concerning cross-contamination risk for the clinicians who share them.
The article concludes that a promising solution for infection protection for the stethoscope is the use of aseptic disposable diaphragm barriers. The authors cite a recent study of the AseptiScope DiskCover™ barriers (Mayo Clin Proc Innov Qual Outcomes. 2020. doi:10.1016 / j.mayocpiqo.2019.10.010), which concluded that barrier use provided protection against common hospital-associated pathogens including MRSA, VRE, and E. Coli.
“The application of single-use aseptic stethoscope barriers is emerging as the first practical solution to this long-standing challenge,” said Scott Mader, CEO and President of AseptiScope. “The upcoming launch of the touch-free DiskCover System will allow healthcare providers to safely and confidently use their most frequently employed medical device, the stethoscope, at a time when infection control is the paramount priority.”
About AseptiScope, Inc.
AseptiScope is a privately funded San Diego, California based, clinical innovation company, formed in early 2016. The organization is founded and led by clinical innovation experts, leading medical researchers and practicing physicians. The AseptiScope mission is to design, develop, manufacture and commercialize novel solutions that ensure “Infection Protection for Clinician & Patient.” The company will introduce the first true and practical solution for the longstanding challenge of stethoscope contamination in the summer of 2020: The AseptiScope DiskCover System. Visit www.aseptiscope.com for more information.
AseptiScope, DiskCover, and related logos are trademarks of AseptiScope, Inc.
MEDIA CONTACT
Irene Mulonni
irene@mulonni.com
858-859-7001